Mental Health Progress Notes
Not sure what mental health progress notes are supposed to look like? Wondering what information to include and leave out? Maybe you’ve heard of psychotherapy notes and are wondering if progress notes are the same thing.
In fact, progress notes are distinct from psychotherapy notes. They have their own role in the practice, which is to provide a baseline of information for other providers (and your patients themselves) to look at regarding your client’s mental health journey.
Read on for insight into mental health progress notes documentation and examples.
What Are Mental Health Progress Notes?
Progress notes record information about a patient’s diagnosis, treatment, sessions, and the overall trajectory of their recovery. Progress notes become part of the patient’s medical record with your practice and may be viewed by other mental or physical healthcare providers as needed. They’re also used by insurance companies to verify what kinds of treatment you deliver and how effective it is for your clients.
Progress notes usually contain information on symptoms, diagnosis, medications, medical history, test results, treatment planning, progress since previous appointment, and a very general overview of the discussion during the session.
Keep in mind that progress notes are different from psychotherapy notes. Psychotherapy notes are private records to be used only by the mental health provider administering the treatment session. They contain information and impressions that might not be appropriate for others to see, such as sensitive personal details the patient has disclosed, the therapist’s private opinion of the patient’s behavior, or areas of conversation the therapist wants to remember to explore next time.
When you write a progress note, you’re writing something that other providers and the patient may see. When you write a psychotherapy note, you’re writing something private for your own reference later.
How Do You Write A Progress Note?
Most progress notes share a basis of common information. You’ll want to check on the exact requirements according to your state licensing board and any professional organizations to which you belong to make sure that you record everything necessary. But in general, here’s how you write a progress note.
- Start with basic identifying information like the client’s name, provider name, and date and location of treatment session. Record how long the session took. You’ll also want to include the patients’ diagnoses and any applicable service codes.
- Test results and prescribed medication should also be logged in progress notes. Capture any information about medication side effects and/or whether it seems to be affecting the patients’ symptoms.
- Record your patient’s current condition. This includes what they tell you about their symptoms and about their state of mind. But also look at their mood, actions, and appearance during the visit to gain more insight.
- If there are issues that may affect your patient’s safety, like suicidal thoughts or an unsafe living environment, you must include them in the note.
- Make general notes about your conversation with your patient during the visit. You need not go in-depth with personal information or details. In fact, it may be best to save that for the psychotherapy notes.
- Talk about the client’s treatment plan moving forward. What is the intended direction of treatment? What seems to be working or not working, and do you need to try a new intervention strategy? You should include the original treatment plan goals as your benchmark to make sure you’re moving in the right direction.
- Finally, don’t forget your signature.
That covers the basic content of a progress note. But you need a plan for how to actually write them. It’s tricky to capture all the relevant information during an appointment while the client is talking to you, but a couple of strategies can help.
Get a Personalized Live Demo
We would love to show you how Valant can help your practice.
Request a Price Quote
Let’s work together to build a package that will accommodate your needs.
Using an EHR
EHRs designed for behavioral health providers will likely offer some sort of template for progress notes so you can write them directly in the EHR. It’s important to find an EHR with features that make the process quick and easy, like:
- Check box format to help you record more information with just a few clicks
- Mental health progress notes templates within the system
- A carry-over feature from previous notes, so you can start each note with unchanging information
- Auto-generated narratives that you can use and edit as needed.
All of these features will save you time. One of the distinct advantages to recording therapy notes in an EHR is that they are secure, as long as the EHR is designed to be HIPAA compliant. The notes don’t sit around your office and you don’t have to remember to lock them in a filing cabinet.
Physical Paper Notes
Some therapists prefer to take notes on paper, as it can feel more natural to jot during a session than to turn to a computer screen while the patient is talking. Some start their progress notes in the computer system, use paper to jot down supplemental information during the meeting, and add the notes manually afterwards, either by typing them up or scanning the notes and attaching the scan to the note.
If you go the physical paper route, you want to make sure that your notes are readable and that they stay secure according to HIPAA requirements from the moment that you make them.
Sample of Progress Notes
Here’s what a progress note written in Valant might look like. Keep in mind, this is only one of several possible templates that can help you capture what goes on during a session.
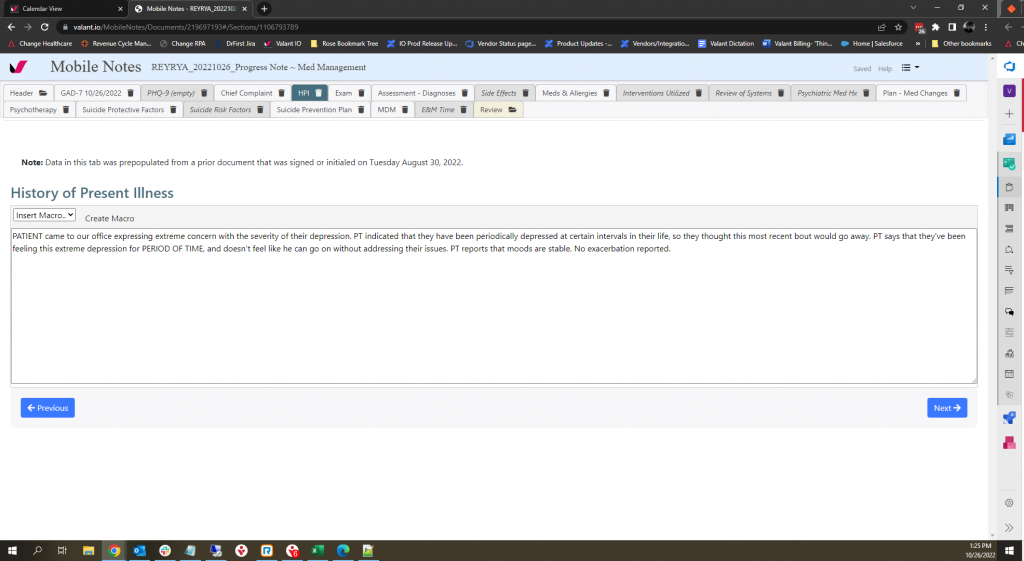
mental health progress notes example
No matter what format you choose for your notes, accurate information is your highest goal. Find the note-taking system that is most efficient and reliable for you, whether that’s an EHR or a notepad.
Related Resources

Put Growth Into Practice: Valant’s Vision for Behavioral Health Success

Celebrating a Year of Shared Success









