Integrated Clearinghouse Features
99%+ Clean Claims Rate
Get paid faster with industry-leading 99%+ clean claims rate, minimizing claim rejections and resubmissions.
5K+ Payer Connections
Connect with over 5,000 commercial and government payers through clearinghouses integrated with your EHR.
White Glove Enrollment
Implement payer enrollments with ease through a guided process from start through go-live.
Batch Eligibility Checking
Skip the tedious manual checks while preventing claim denials by running batch eligibility checks to verify coverage of multiple patients at once.
Easy Claim Submissions
Speed your claims process by submit multiple claims at once directly from your EHR.
ERA Workflow Management
Reduce manual entries and errors in payment posting by receiving ERAs and mapping to patient claims directly in your EHR.
Clear Up Your Billing Bottlenecks
with an Integrated Clearinghouse
Focus your billing efforts on valuable work over tedious tasks. By running billing through your EHR, you eliminate manual claim exports and remittance uploads, reduce eligibility errors, and gain insight on your entire revenue cycle.
How Clearinghouses Work For You
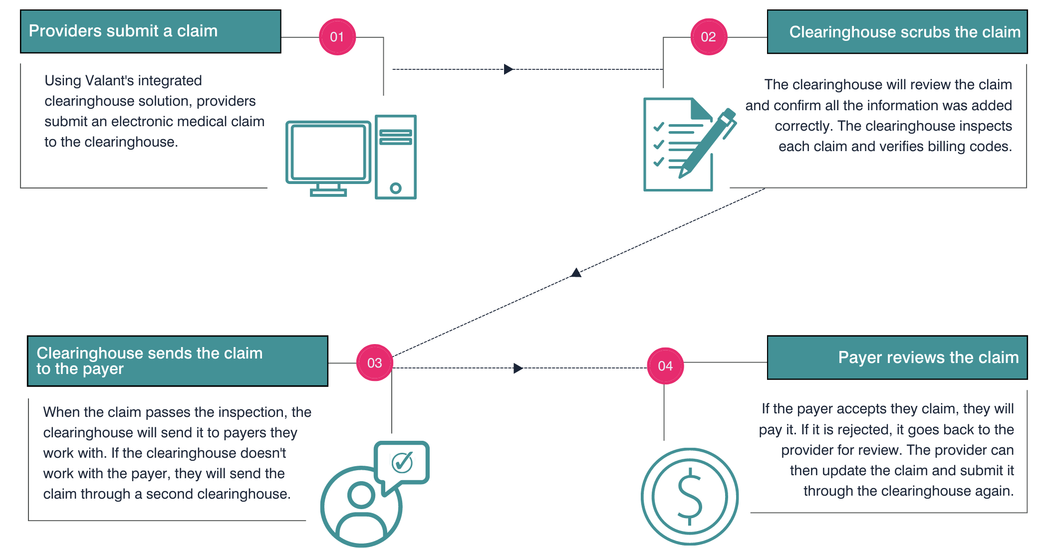
You can get the reimbursements you deserve and avoid payment delays or denials when a clearinghouse act as the bridge between your practice and insurance companies by checking claims for errors before sending to payers.”


Get A Clearinghouse That Goes Above & Beyond
Good clearinghouse partners give decent payer connections, scrub claim errors, and verify billing codes. Great clearinghouse partners give expansive payer connections, improve clean claims rate, and make it easy to track submitted claims and follow up with insurance companies so you get paid.
Top Clearinghouse Options for Behavioral Health
Gain confidence in clean claim submissions and timely remittance with top-tier clearinghouse partners integrated with your EHR.
Talk with our team today to about what you can do with an integrated clearinghouse through Valant.


Be the Hero of Your Billing Team
Access top-rated clearinghouse partners dedicated to serving the needs of behavioral health practices. With integrated clearinghouse options through Waystar and Optum that make claim submission easy, check errors for you, and deliver detailed remittance advice, your billing team will thank you.”
Receive More Payments with a 99%+ First-Pass Rate
Send claims with confidence that they won’t bounce back when you can get a 99%+ first-pass rate for all submitted claims. How much time could your practice save on wrestling with insurance companies over rejections?
Speed Your Revenue Cycle to Invest In Your Practice
Get your payments schedule into a regular cadence when most of your claims clear on the first try. By improving your cash flow, you can better project revenue and invest in your practice with confidence.
Make Appeals Easy When Denials Happen
Create headache-free appeals with 1k+ pre-populated payer-specific appeal forms. Reduce your cost to collect when you submit up to 100 appeals in a single batch through Waystar’s Appeal Wizard.
Free Up Time with EHR-Integrated Clearinghouses
Refocus your revenue cycle efforts by letting a clearinghouse partner handle the tedious work of checking, cleaning, and ensuring claims are sent to the right payers in the right format. Just submit claims through your EHR and let your clearinghouse handle the rest.
Integrated Clearinghouse Solution
How Billing With a Clearinghouse Works
See Other Ways Valant Can Improve Your Administrative Efficiency
What They’re Saying
Integrated Clearinghouse Solution
Related Resources

Why Your Practice Should Accept Insurance for Therapy Along With Private Pay




